Healthcare systems face mounting strain due to aging populations, chronic disease growth, and rising expectations for service quality.
Innovation offers a path to improve sustainability, cut operational waste, and enhance care outcomes.
Digital tools, AI, and remote care models reshape service delivery and help organizations modernize.
The seven practical strategies below outline how providers can accelerate progress using proven methods and measurable results.
1. Leverage Digital Technologies for Process Efficiency

Hospitals continue to improve operational performance by adopting digital tools that enhance coordination and reduce avoidable delays.
Many facilities report substantial reductions in average length of stay due to refined clinical process management strategies.
Mobile communication platforms further support immediate collaboration among clinicians, accelerating diagnostic decisions and improving responsiveness during urgent cases.
EHR usage across the United States has reached very high adoption levels, allowing faster retrieval of patient information and more reliable documentation practices.
Modern AI-driven documentation assistants, including voice-enabled note-taking systems, relieve clinicians of time-consuming administrative work and help them maintain focus on direct patient interaction.
Data highlighting these gains in efficiency reveals measurable operational improvements:
- Average hospital stay reductions of roughly one-third in some organizations
- EHR adoption rates above eighty percent among U.S. physicians
Digital workflows extend these gains across scheduling, billing, and internal communication.
Automated routing reduces bottlenecks, while integrated dashboards give staff clearer insight into daily activity.
Facilities benefit from smoother patient movement through each stage of care and more consistent handoffs between departments.
2. Enhance Access Through Telehealth and Remote Care
Telehealth lifts geographic constraints and creates pathways for patients who face challenges securing in-person care.
Rural communities often struggle with provider shortages, long travel times, and limited specialty access, so remote connections play a vital role in closing service gaps.
Patients gain easier access to clinicians through video visits, secure chats, and remote monitoring tools that support ongoing care without unnecessary trips.
Platforms offering same-day or next-day appointments illustrate how digital access can expand availability and reduce delays.
Mental health services delivered through text-based environments show strong performance in reaching individuals who might avoid traditional sessions due to stigma, scheduling issues, or mobility limitations.
Data reflecting the impact of remote interventions contributes important context:
- Reductions of about 31% in hospital admissions have been reported under structured telehealth programs.
- Decreases of about 48% in hospital days further reinforce the value of continuous remote support.
Remote care strengthens adherence, improves care continuity, and gives patients more flexible options to engage with providers.
3. Empower Patients with Self-Monitoring and Control Tools
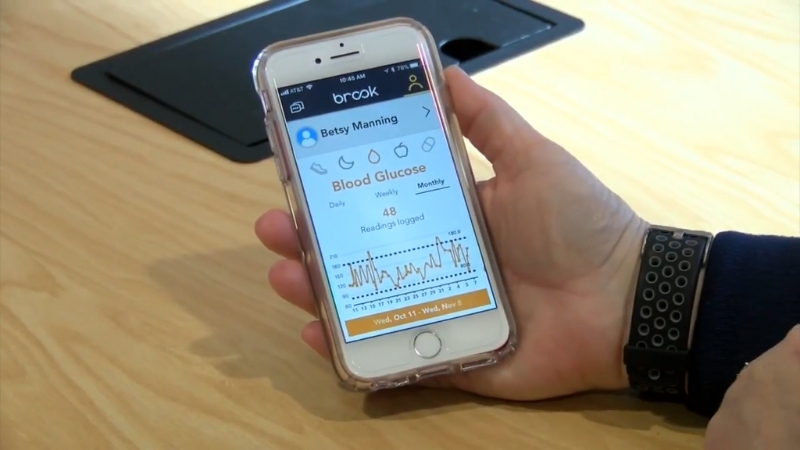
Patients increasingly rely on self-monitoring applications to manage chronic conditions, track lifestyle choices, and monitor biometric data.
Apps designed for diabetes care, weight management, or cardiovascular risk provide dashboards for daily logging, trend analysis, and personalized goals.
Coaching components offer human guidance, reinforcing habits that sustain long-term improvement.
Digital tools geared toward patient autonomy reduce congestion in clinics and streamline routine visits.
Online check-ins and automated alerts shorten waiting times during busy hours, allowing staff to distribute workload more efficiently.
Home monitoring devices, including glucometers, blood pressure cuffs, and activity sensors, send data directly to care teams for early review.
Patients benefit from greater control, fewer disruptions, and increased confidence in daily health management.
Innovative wellness therapies such as the bariatric chamber Los Angeles offer a supportive healing environment that boosts oxygen delivery at the cellular level, promoting tissue repair and overall recovery.
4. Integrate Artificial Intelligence for Predictive and Personalized Care
View this post on Instagram
AI brings a forward-looking approach to clinical decision-making by identifying risks before problems escalate.
Predictive models analyze large datasets to highlight early signs of deterioration, flag gaps in treatment, and guide clinicians toward timely interventions.
Conditions that once went unnoticed until symptoms intensified can now be spotted earlier, improving chances for successful outcomes.
Personalized care gains strength as AI interprets patterns across patient histories, genomics, and treatment responses.
Providers adjust therapy with more precision, reduce unnecessary tests, and anticipate resource needs.
AI-supported triage tools further optimize operations by guiding teams on case priority and coordination.
5. Promote Inclusive and Culturally Competent Communication

Communication errors contribute heavily to clinical risk, so dependable communication systems serve as an essential foundation for safe care.
Multilingual translation platforms allow clinicians to communicate accurately with patients who speak different languages, eliminating dependence on family members who may lack medical vocabulary.
Sensitive conversations become more accurate and less stressful for all involved.
Captioning tools that support real-time subtitles for patients with hearing impairments, and secure voice-activated assistants make health information more accessible to individuals who prefer verbal interaction.
Staff also rely on these systems to ensure instructions are clear, consistent, and aligned with cultural expectations.
Important data emphasizing the influence of communication challenges includes:
Culturally responsive communication strengthens trust, increases patient participation, and improves adherence to care plans.
6. Strengthen Coordination via Health Information Exchange
@dr_jen_naynay Confidentiality concerns with Health Information Exchange. #patientadvocacy #tiktokforgood #healthcarereform #tiktokdocs #doctorsoftiktok #secondopinion #medicalgaslighting #chronicillness #primarycare #osteopathicmedicine #hipaa #duetwithme ♬ original sound – dr_jen_naynay
Health Information Exchange platforms offer secure pathways for sharing patient records across various sites of care.
Clinicians accessing HIE systems receive instant visibility into medication history, diagnostic tests, and prior treatments.
Better insight into patient background reduces duplicate testing and enhances care quality.
Complex cases involving multiple specialists benefit greatly from interoperable records.
Each provider gains a clearer picture of ongoing treatments, eliminating delays caused by missing information.
Care transitions between hospital, outpatient clinics, and community partners become smoother when data is available at the moment it is needed.
7. Invest in Training, Remote Staffing, and Organizational Adaptation
Training ensures staff remain confident using modern tools and understand ethical considerations tied to data security, clinical decision support, and virtual engagement.
Online training programs help teams stay aligned with best practices and rapidly emerging clinical standards.
Virtual workshops, short courses, and simulation modules reinforce practical skills without disrupting daily responsibilities.
Remote staffing reduces pressure on traditional workforce models by supporting administrative needs, triage functions, and patient communication tasks.
HIPAA-compliant virtual assistants handle high-volume work such as:
- Scheduling
- Billing
- Insurance coordination
- Documentation preparation
Several meaningful points reveal how staffing modernization supports organizational stability:
- Remote assistants help mitigate shortages by covering essential administrative duties without occupying on-site space.
- Organizations gain scalable capacity, adjusting support levels based on surges in patient demand.
Adaptation of staffing models and training programs creates more resilient operations during fluctuations in volume or resource availability.
The Bottom Line
Innovation in healthcare thrives when technology, process design, and patient engagement move forward together.
Digital systems raise efficiency, telehealth expands access, self-monitoring tools strengthen patient involvement, and AI sharpens clinical foresight.
Inclusive communication and secure data exchange reinforce safety and coordination. Training and remote staffing enable organizations to adapt as pressures grow.
Health systems that adopt these practices position themselves to deliver care that is efficient, accessible, and centered on patient needs.

